Cancer cell ‘memory’ of oxygen deprivation explains tumour spread published: February 9, 2015
Liverpool researcher's have shown that cells, with previous experience of oxygen deprivation, can still produce the genes that help them move around the body.
Scientists at the University of Liverpool have shown that a type of cancer, common in young children, is more likely to spread in the body if the cells have experienced a shortage of oxygen inside the tumour.
The research, in partnership with paediatric oncologists and surgeons at Alder Hey Children’s hospital, highlights the need to monitor the cellular environment in the body to help predict the consequences of the cells’ history on their future behaviour and their potential response to therapies.
Supported by the Neuroblastoma Society, the study shows that neuroblastoma cells, an aggressive cancer that usually occurs in infants and children under the age of five, have a ‘memory’ of oxygen deprivation, a phenomenon which occurs in solid tumours.
Lack of oxygen modifies how the cells behave for a period of time, prompting a change in the expression of specific genes. The consequence is that cells can detach from the tumour mass and spread through the body. They also provide a means for neighbouring cells, which were not deprived of oxygen, to behave in the same way.
Complex process
Some of the genes that are produced as a result of oxygen deprivation make the cells stickier, allowing them to grip the blood vessel walls, escape into the blood circulation, and settle in a new organ of the body.
Dr Violaine See, from the University’s Institute of Integrative Biology, said: “Therapies targeting cancer spread are challenging due to the complexity of the process and the high number of variables involved.
“Although tumours that are deprived of oxygen have previously been associated with increased aggressiveness as well as resistance to treatment, the understanding of a direct link between the level and duration of hypoxia and the individual steps involved in cancer spread was still missing.”
Tailored therapies
Paul Losty, professor of paediatric surgery at Alder Hey Children’s Hospital NHS Foundation Trust, said: “We now know that even those cells that have enough oxygen supply, can ‘remember’ a previous environment where they did not have sufficient oxygen. With this new knowledge, we can look more carefully at therapies tailored to the cellular environment.”
Neuroblastoma is a rare and aggressive childhood cancer, with around 100 children in the UK diagnosed each year.
The research is published in the journal Oncogenesis. For more information about neuroblastoma, please vist: www.neuroblastoma.org.uk.
Cell behaviour in low oxygen conditions mapped published on February 19 2014
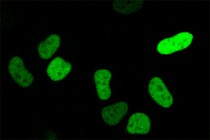
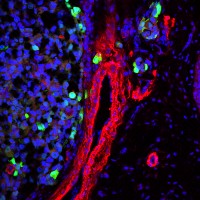
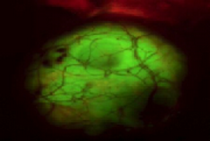
Human cells cultured in low oxygen express a nuclear protein induced by hypoxia in their nuclei. This protein can then switch on specific gene expression. Research at the University of Liverpool has explained how cells behave when placed in a low oxygen environment, a development that could have implications for cancer patients and other serious illnesses.
The research opens up the possibility of controlling the signals that keep cells alive, preventing the damages caused by ischemia – a restriction of blood supply to tissues. It could also work to help destroy cancer cells.
When the body is deprived of adequate oxygen supply it is known as hypoxia and can cause the death of cells. This occurs in patients suffering from ‘ischemia’, which can lead to gangrene or paralysis.
“These findings could have important consequences for how we understand tumours, which are hypoxic because of the rapid cell growth which outpaces their blood supply”A reduction in oxygen levels, such as that used in the new study and which mimics the situation in a tumour, causes cells to adapt to the new environment and become resistant.
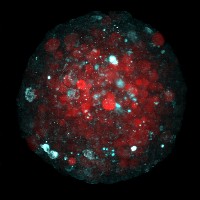
The researchers from the Institute of Integrative Biology in collaboration with researchers from the Department of Mathematical Sciences at the University, subjected cells to conditions with only 1% oxygen for 20 hours, and imaged the cellular response in real-time. They then mathematically modelled the profile of the proteins which conveyed instructions telling the cells how to behave.
It has not been established before why some cells died and others lived under low oxygen conditions, but by monitoring the levels of proteins in the cells and observing how they influenced genes switching on in the cells, the researchers were able to determine the optimum conditions for keeping cells alive.
Cell biologist, Dr Violaine See, who led the project, said: “These findings could have important consequences for how we understand tumours, which are hypoxic because of the rapid cell growth which outpaces their blood supply.”
The study was published in the Journal of Biological Chemistry and was funded by the Biotechnology and Biological Sciences Research Council (BBSRC).
Scientists awarded £1M to advance cell imaging techniques (published on February 22 2013)
Researchers at the University of Liverpool have been awarded £1 million to advance imaging techniques in improving understanding of the processes that occur inside living cells.
The award – part of a £25.5 million investment into microscope technology from the Medical Research Council (MRC), the Biotechnology and Biological Sciences Research Council (BBSRC), and the Engineering and Physical Sciences Research Council (EPSRC) – will contribute towards new microscope technology and expertise to support researchers, the NHS and local biotechnology industries.
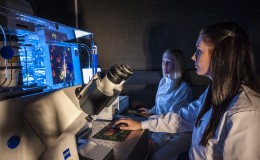
The new generation of imaging techniques are able to greatly increase the resolution when studying an intact and living cell. They allow researchers to study live biological processes as they are taking place at fractions of a second. Visualising these tiny biological structures helps further understanding into the causes of a wide range of diseases
Dr Violaine Sée, from the University’s Centre for Cell Imaging, said: “This funding will help advance research into areas such as cancer, ageing, infectious disease and the development of nanomedicines. Researchers will now benefit from the latest imaging technologies to investigate cellular events at the molecular level as they unfold in real time.”
Dr Raphael Levy, from the University’s Institute of Integrative Biology, said: “Funding at Liverpool will contribute to two new state-of-the-art microscopes for fluorescence detection inside living cells and small organisms. It will also allow for the upgrade of a unique custom-made microscope specifically designed for imaging nanoparticles inside cells.
“Using these new technologies scientists will be able to progress study into areas such as the resistance of malignant cells to anticancer drugs. New technologies will help us better understand the dynamic interaction of man-made nanoparticles with living cells.”